Breadcrumb
Keeping Cancer Care Close to Home
By Jennifer New
Published on June 7, 2024
The Iowa Cancer Affiliate Network helps community hospitals provide enhanced levels of cancer care to rural patients.
Cancer patients have days when it’s easier to feel nearly “normal,” and others when physical pain and emotional distress are overwhelming. These harder days often coincide with challenging treatments like chemotherapy and radiation. Even seemingly routine oncology appointments can elicit doubt and confusion.
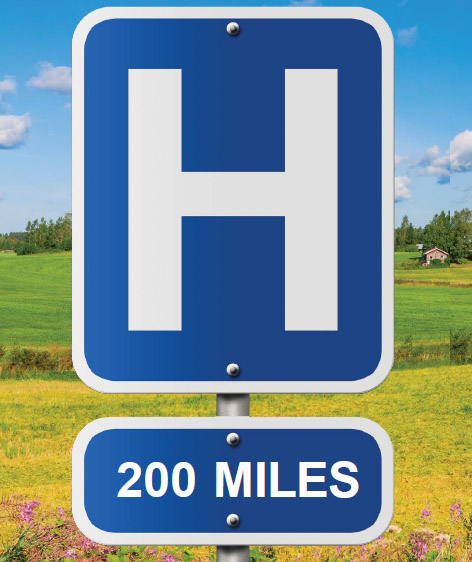
The bottom line is that cancer treatment is rough, riddled with affronts to the body and complex challenges to the psyche. What makes it easier to navigate is being able to sleep in one’s own bed, having loved ones nearby, and receiving advice from trusted and familiar doctors. For too many rural
Iowans, however, cancer treatment means long hours in the car and visits to unfamiliar people and places.
Enhancing Community Cancer Care
Amy Fernandez, the chief of clinic services at Mahaska Health in Oskaloosa, Iowa, knows how hard this can be on patients. An experience she had as part of a friend’s caretaking team inspires her to work to improve rural cancer care.
“We would drive three hours total to and from [the hospital],” she recalls of their trips to University of Iowa Health Care in Iowa City. “He was so sick on the way home. I’d try to drive as carefully as I could, and sometimes we’d have to pull over. I can’t help but think how much easier it would have been on him to drive 20 minutes to a local hospital.”
This is exactly the intention of the Iowa Cancer Affiliate Network (I-CAN). Established three years ago with funding from the National Cancer Institute, a part of the National Institutes of Health, I-CAN is a conglomerate of hospitals that work together to provide enhanced levels of care to cancer patients. It is coordinated by researchers and staff in the University of Iowa (UI) College of Public Health, the Holden Comprehensive Cancer Center at UI Health Care, and the Carver College of Medicine, under the leadership of Mary Charlton, professor of epidemiology. Charlton stresses that they are building a collaborative approach that focuses on all levels of cancer care, “from dietary needs to access to national trials.”
Charlton and members of the I-CAN team were inspired by a network approach spearheaded at the University of Kentucky. In a state that has a similar rural-to-urban composition, the Markey Cancer Center Affiliate Network program has grown to include 19 community hospitals and medical centers. In 2023, I-CAN members traveled to Kentucky to learn how they established and continue to maintain their network.
Dave Evans, the clinic manager at the Southeast Iowa Regional Medical Center in West Burlington, was part of that trip. “I got to meet people who have similar-sized health systems to us. It was very helpful to see their workflows.”
Evans says that in the past, he and his colleagues worried about competing with other hospitals, especially larger ones. Last year, Southeast Iowa Regional Medical Center provided chemotherapy to about 800 patients. By comparison, a large hospital might provide chemotherapy to thousands of patients each year. With I-CAN, however, everyone is on the same team. “It’s a true partnership,” says Evans.

Reducing Rural Cancer Disparities
Working together to combat Iowa’s dire cancer numbers is at the heart of I-CAN. As Charlton points out, “Iowa has the second highest cancer rate in the country, and we know that rural patients fare less well than their urban counterparts.” By combining the strengths of a research hospital that has access to the latest information, technology, treatment trials, and more, with the strengths of rural hospitals, the hope is to shift the disparity of outcomes.
There are myriad benefits to keeping patients in their home health care facilities. An important one is that it’s easier to involve family and friends in caretaking and appointments. Also, some patients are much more likely to accept treatment advice from trusted, long-term providers.
I-CAN also focuses on benefits that are less visible to patients, such as connecting providers in the network to training and guidance from team members in Iowa City, and via them, to the international oncology community. In addition, I-CAN works in collaboration with the Iowa Cancer Registry, which is directed by Charlton, to help build infrastructure for data collection and monitoring in network hospitals.
“We worked with the UI to do a gap analysis,” says Fernandez, “determining what services we have available and what we’re missing. We decided to get two of our people trained as tumor registrars, and we’re now seeing about a hundred patients a year for tumor analysis.”
She says that this hands-on approach to data collection is helping them to hone their understanding of the local situation: “When we first looked at statistics for Mahaska County, cases were being diagnosed later here than in other parts of the state.”
Mahaska Health is the smallest of the six rural medical centers that are part of I-CAN. Today, Fernandez is excited by the breadth of services and information they can provide. “At a hospital our size,” she says, “we don’t have a geneticist, but now we have access to this—someone who is encouraging testing for the patient and family members. And instead of one oncologist looking for trials and the latest research, we have access to an entire team focused on it.”
Learning Opportunities
One of the people who visited Mahaska Health at an initial meeting is Madi Wahlen, an MD/PhD candidate in the Medical Scientist Training Program at the UI. She coordinates I-CAN’s research activities and facilitates data collection.
“It’s a very small hospital, but close to 20 people showed up for that first meeting,” Wahlen remembers, adding that although their annual number of cancer patients is relatively small, “their passion for improving the level of care was so impressive.”
As a student, Wahlen has had the unique opportunity to attend the meeting in Kentucky and visit all six of the network hospitals. Learning how hospitals work is not directly taught in medical school. “I’ve really been able to understand the strengths of small hospitals,” says the Minnesota native, “as well as the bandwidth issues they face.”
The project has also afforded firsthand experience in implementation science, which is at the heart of I-CAN. This developing field studies why interventions, such as diet or exercise, are or are not successful. “You can have the best intervention on paper, but if you don’t facilitate it well and people don’t do it, then it doesn’t matter,” Wahlen explains.
Sharing Resources
A key goal of I-CAN is to have all members successfully implement the evidence-based quality practices and protocols set forth by the American College of Surgeons Commission on Cancer (CoC), the standard-setting consortium. “The amount of resources required to meet the CoC standards favor larger hospitals that tend to be located in urban areas. We want to share resources so that smaller hospitals located in rural areas can achieve CoC standards,” says Charlton.
The effect is a win-win. Hospitals like Evans’ in West Burlington now have tumor boards, in which “a team sits down and discusses scans to establish a plan of care before treatment has even begun.” While at Mahaska Health, patients work with cancer navigators who help meet their psycho-social needs, such as finding quality wigs or a prosthetics provider.
“Cancer has affected us all in one way or another,” says Fernandez. “Through I-CAN, we’re expanding our footprint while keeping care close to home.”
This story originally appeared in the spring 2024 issue of InSight.